Help Others Discover – Click to Share!
When discussing digital healthcare records, you may have heard the terms EHR (electronic health record) and EMR (electronic medical record) used interchangeably. At first glance, the difference seems so small, just a single letter, but that letter indicates a vast difference in the spectrum, intention, and patient care delivery.
Across the world, adoption of digital software for patients records and other factors is steadily increasing. The World Health Organisation states that over 80–90% of hospitals and providers in higher-income nations are using some form of electronic record, however adoption is lower in middle- and low-income countries. Across the world, hundreds of hospitals and tens of thousands of hospital beds are being managed by EHR/EMR systems, although full interoperability is an ongoing process.
In the UK, this digital shift is happening too; 94% of NHS trusts and 97% of GP practices are using an digital health records system in the form of either EHR or EMR, and over 12.25 million distinct users have control over their health records through the NHS App, all signalling a genuine move towards patient-centred, connected care and patient access.
Recent studies highlight that AI-powered EHR solutions are significantly improving efficiency and patient safety across healthcare systems globally and in the UK. Around 90% of clinicians using AI-integrated EHRs report improved operational efficiency, with 60% saving up to four hours daily on documentation. Research also shows administrative overheads reduced by about 35%, while documentation time dropped from 4.3 to 1.8 hours per day with advanced digital systems. Hospitals using analytics-driven EHRs have achieved 10–20% savings in resource allocation, improved bed utilisation, and shorter wait times. On the safety front, EHR adoption has been linked to a 46% reduction in medication errors and up to 30% fewer diagnostic errors, while AI integration has further reduced medication error rates to nearly 2% and cut patient wait times by 13–17 minutes. Additionally, organisations leveraging regulatory analytics reported a 63% drop in compliance-related incidents, underscoring the dual benefit of AI in boosting efficiency and clinical safety.
These adoption milestones are closely aligned with the NHS Long Term Plan (10-Year Plan), which places digital transformation at its centre. The plan aims for both the clinical and non-clinical activities within NHS trusts to be fully digitised by 2026, enabling clinicians to obtain accurate and real-time patient data across care settings and giving patients more control to have access to their own health records. The NHS 10-Year plan makes clear the importance of both EHRs and EMRs in delivering integrated, efficient and high-quality health care across the UK by focusing on interoperability, secure data sharing, and patient-centred digital services.
Understanding EHR vs. EMR isn’t just about definitions; it’s about recognising how the right system can shape the future of healthcare delivery.
An Electronic Medical Record (EMR) is a digital version of a patient’s chart within a single clinician’s office. Think of it as a modern version of all those big, thick folders being stocked away on clinic shelves.
Key Features of EMRs:
Advantages of EMR:
EMRs work best for smaller practices looking to digitise internal records, but the data typically doesn’t travel beyond the healthcare facility.
An Electronic Health Record (EHR), on the other hand, is much broader. An EHR is a comprehensive, digital version of a patient’s health information that is designed to be shared securely across multiple healthcare providers and organisations. This makes EHRs particularly valuable in today’s connected care environment.
Features of EHRs:
Benefits of EHRs:
Aspect | EMR (Electronic Medical Record) | EHR (Electronic Health Record) |
Scope | Records within one practice | Records across multiple providers & systems |
Data Sharing | Limited or none | Designed for interoperability |
Patient Focus | Practice-centric | Patient-centric, longitudinal |
Use Case | Clinical workflow, billing, in-clinic use | Coordinated care, telehealth, population health |
Access | Providers in one clinic | Providers, patients, and authorised stakeholders |
If EMR is practice-centric, EHR is patient-centric. This is the reason the EHR vs EMR distinction is relevant to today’s connected healthcare ecosystem.
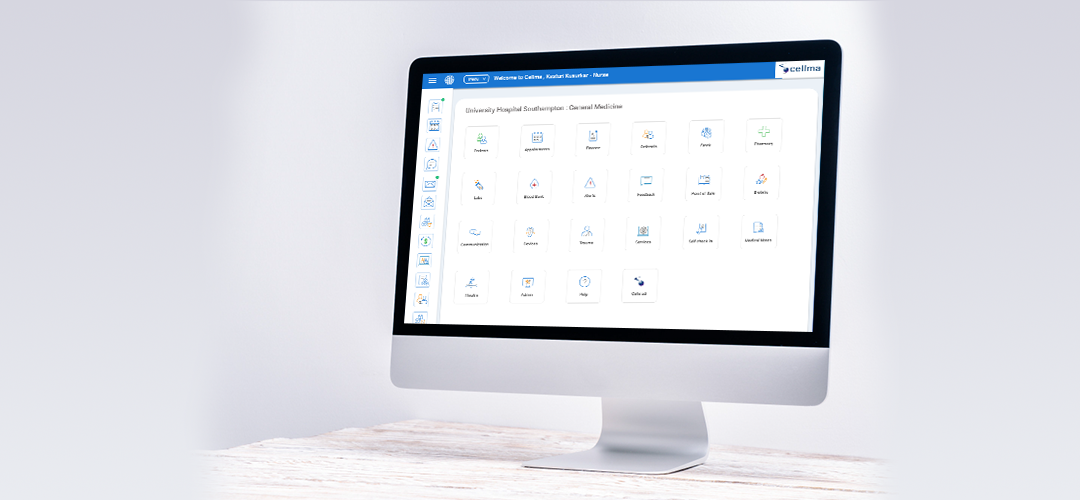
At RioMed, we designed Cellma to bridge the gap in the EHR vs. EMR conversation by offering a single platform that adapts seamlessly to both needs. Whether a practice is looking for an EMR to manage patient records internally, or a healthcare system requires a fully interoperable EHR to connect providers, Cellma delivers a comprehensive, modular solution.
Modular Design for All Care Settings:
Cellma is a comprehensive modular platform facilitating the entire patient journey across 30+ specialties. Key modules include:
Interoperability by Design:
Cellma has interoperability at its core so it can work across local, regional, national, and even across global health systems. Whether deployed in an NHS organisation or an international health system, Cellma allows data to flow securely, and efficiently across care settings, use both NHS specific, and global interoperability standards.
Supports NHS Interoperability Requirements:
GP Connect – Enables direct and secure sharing of information with general practices.
Shared Care Records – Enables shared patient information across NHS organizations.
CIS2 (Care Identity Service 2) – Provides secure authentication for NHS users.
PDS (Personal Demographics Service) – Verifies the accuracy of patient details and demographic information.
Supports Global Interoperability Standards:
FHIR (Fast Healthcare Interoperability Resources) – A modern API structure for sharing discrete data about health.
HL7 – A standard for exchanging clinical and administrative patient data across health sector applications.
DICOM – Provides the means to transfer and manage medical imaging information.
SNOMED CT – A comprehensive clinical terminology for consistent coding and analysis of data on a worldwide basis.
Through adherence to both NHS and international interoperability standards, Cellma equips providers with the ability to offer coordinated, connected and compliant care – anywhere in the world.
Strong Compliance Framework:
Cellma stands on trust as an organisation, complying with rigorous NHS and global regulatory frameworks to provide and deliver safe, secure and compliant healthcare services. Our strong compliance enables safe and secure patient data, supports ethical clinical practices, and meets international standards for the quality and security of healthcare.
NHS Compliance Frameworks that Cellma supports:
GDPR (General Data Protection Regulation) – Privacy and protection around patient data.
NICE guidelines (UK) – Supports clinical workflows complying with NHS standards of evidence-based practice.
NHS DSP Toolkit – Evidence of compliance with NHS data security and protection controls.
Cyber Essentials Plus Certification – Evidence of security controls, such as cybersecurity and data protection.
Conform with Global Compliance Elements:
Risk Ledger Assurance – Increases transparency and security in the supply chain.
ISO 9001 (Quality Management System) – Provides assurance of consistency in quality.
ISO 14001 (Environmental Management System) – Supports sustainable and environmentally responsible practices.
ISO 27001 (Information Security Management System) – Safeguards sensitive health information through internationally acknowledged information security processes.
By staying aligned with both NHS and international compliance frameworks, Cellma enables healthcare organisations across the globe to operate with confidence, security, and total regulatory compliance.
Security & Patient Safety:
Security is central to Cellma with end-to-end encryption, role-based access controls, and robust audit trails. Cellma meets compliance requirements and also uses AI safety tools to support patient safety:
Demonstrated Success in Relevant Experience
Cellma has already been successfully implemented across healthcare systems from all corners of the globe and is used in high-pressure environments like emergency departments, national screening programmes, community health, occupational health and specialist clinic settings. This fact ensures that Cellma is as effective in a single-site clinic, multi-site organisational operations, or in a health infrastructure of a complete country.
Cellma is more than just an EHR or EMR; it’s a future-ready healthcare platform. Cellma combines interoperability, compliance, security and applicability of AI-enabled innovative tools in a way that facilitates the need to focus on patient care, with the assurance that records are accurate, linked and protected.
The whole EHR vs. EMR conversation involves far more than semantics; it’s about how care is delivered now and in the future. While EMRs focus on digitising records within a practice, EHRs open the door to collaboration, interoperability, and truly connected patient care. But why settle for one when you can have both?
With Cellma, you can have it all. It’s a platform designed to deliver the day-to-day efficiency of an EMR while providing the interoperability and compliance of a world-class EHR. Whatever your requirement is, small clinic or a national health authority, Cellma can be tailored to your requirements, enabling clinicians and improving patient experience in every setting.
Future-ready healthcare starts here. Book your free Cellma demonstration.
Recent Blogs
Let’s transform healthcare together. Speak with RioMed for a tailored solution.
Yes. Cellma is designed to work as both EMR and EHR; as an EMR it can support clinics with internal workflows e.g., charting, billing and patient care, whilst providing healthcare ecosystems with full interoperability through national and international interoperability standard connections e.g., FHIR, HL7 and GP Connect and Shared Care Records; therefore Cellma can be considered both an EMR and EHR both.
Cellma is built with strict adherence to global healthcare standards and regulations. It complies with GDPR, NHS DSP Toolkit, NICE guidelines, Cyber Essentials Plus, and ISO certifications (ISO 9001, ISO 14001, ISO 27001). Globally, Cellma adheres to international frameworks such as ISO 9001 (Quality Management), ISO 14001 (Environmental Management), and ISO 27001 (Information Security Management) to maintain consistent, secure, and ethical data handling across all regions.
Security features include end-to-end encryption, role-based access, and full audit trails, so patient data is always secure.
Whereas many solutions offer only EMR or EHR capabilities, Cellma offers both. In fact, it is modular and has over 30 specialties covered. Cellma offers a range of tools such as PAS, EPR, Document Management, e-Pharmacy, Lab & Imaging integrations, and advanced BI reporting. What truly sets Cellma apart is its scalability - it’s not just adaptable in theory, but proven in practice. Whether deployed in a single clinic, a regional network, or a national health system, Cellma flexes effortlessly to meet the needs of any healthcare organisation.
The fact that it leverages AI-powered insights and predictive analytics, and has proven extensive use in complex, demanding situations such as Emergency Departments. Cellma stands out as a future-ready healthcare platform.